Hyperemesis Gravidarum
Introduction:
Pregnancy is a wonderful and changing time in a woman’s life. This magnificent journey, however, might be overshadowed for some pregnant moms by a disease known as hyperemesis gravidarum. Hyperemesis gravidarum, an uncommon name, refers to a severe kind of morning sickness that affects only a small number of pregnant women. We go deeper into the nuances of hyperemesis gravidarum in this article, giving light on its symptoms, causes, and potential therapies.
What is Hyperemesis gravidarum?
Hyperemesis Gravidarum is a disorder that affects pregnant women during their pregnancy. In contrast to typical morning sickness, which usually decreases during the first trimester, hyperemesis gravidarum is distinguished by continuous and severe nausea and vomiting. This condition can have a significant influence on the mother’s general well-being, necessitating medical attention and assistance. HG is a severe and persistent condition of nausea and vomiting during pregnancy. While most women have mild morning sickness, which usually subsides during the first trimester, those suffering with hyperemesis gravidarum experience extreme and chronic nausea and vomiting. These symptoms can cause severe dehydration, decreased weight gain, and even starvation, putting both the mother and the infant at risk.
What causes Hyperemesis gravidarum?
While the precise etiology of hyperemesis gravidarum is unknown, various theories claim that it is caused by a mix of genetic, hormonal, and psychological factors. The rapid rise in pregnancy hormones, particularly human chorionic gonadotropin (hCG), is thought to be important in triggering and aggravating symptoms. A family history of hyperemesis gravidarum or a previous condition like as gastroesophageal reflux disease (GERD) might also contribute to the development of HG.The specific cause of hyperemesis gravidarum is yet unknown. However, evidence indicates that hormonal changes, specifically an increase in human chorionic gonadotropin (hCG) levels, may have a substantial effect. Other factors that may contribute to hyperemesis gravidarum development include:
- Predisposition due to genetics
- Thyroid function changes
- Disorders of the gastrointestinal tract
- Deficiencies in vitamins
- It is important to highlight that each woman’s experience with hyperemesis gravidarum will differ, and further research is needed to properly understand its varied underlying causes.
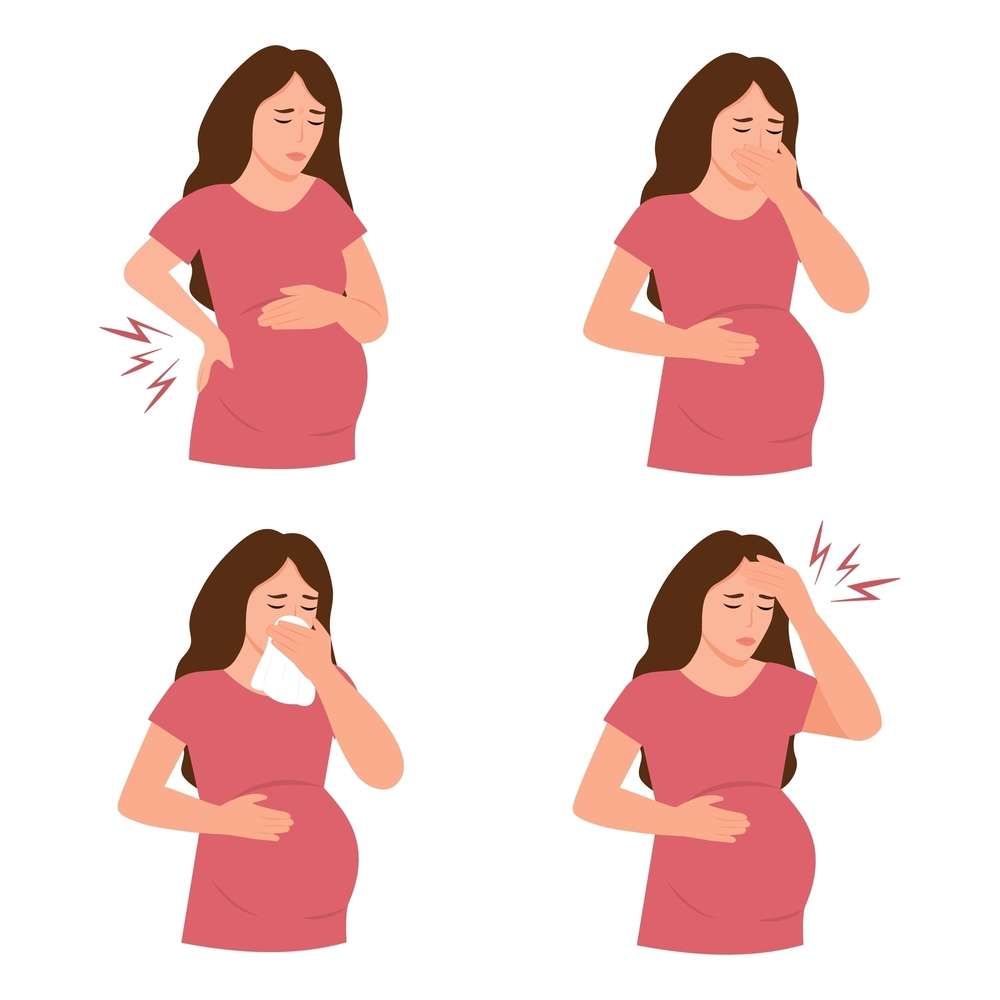
Symptoms of hyperemesis gravidarum:
Recognizing hyperemesis gravidarum symptoms might assist women in seeking appropriate medical care. Here are some frequent warning signs and symptoms to look out for:
- Severe and long-lasting nausea and vomiting
- inability to keep meals and fluids down
- Weight loss that is significant
- Dehydration can be identified by dark urine or infrequent urinating.
- Constant feelings of exhaustion and weakness
- Feeling dizzy or fainting episodes
- To receive quick examination and treatment, it is critical to be proactive and report any worrying symptoms with your doctor.
Prevalence:
Although uncommon, hyperemesis gravidarum affects roughly 0.5-2% of pregnant women. It is particularly common in first-time mothers, women carrying multiple kids, or those who have a history of headaches or motion sickness. Understanding the prevalence and risk factors for HG enables healthcare providers to identify women who may be at higher risk and provide the necessary support.
Hormonal Factors:
Hormonal changes are unavoidable during pregnancy, and it is assumed that an imbalance may contribute to hyperemesis gravidarum. Hormone surges like as estrogen and progesterone have the ability to disturb the body’s regular gastrointestinal functioning, resulting in chronic nausea and vomiting.
Psychological Aspects:
Hyperemesis gravidarum has also been linked to psychological issues such as increased stress and anxiety. The emotional toll of living with the condition can aggravate symptoms and make them more difficult to control. As a result, emotional support and therapy are critical for women suffering from HG.
Genetic Factors:
Genetics may have a role in hyperemesis gravidarum, according to research, because the disorder commonly runs in families. Genetic variations that may enhance the risk of HG have been identified in studies, providing vital insights into potential future therapeutics. More research, however, is required to completely understand the intricate interplay between genetics and hyperemesis gravidarum.
Hyperemesis Gravidarum: When to Go to the Hospital?
It is critical to understand when to seek medical attention if you are suffering symptoms of hyperemesis gravidarum. While some nausea and vomiting are common during pregnancy, it is critical to detect when it becomes excessive. If you are unable to keep any food or water down for more than 24 hours, you should consider going to the hospital.
- You are either losing weight or becoming dehydrated.
- You get lightheadedness, dizziness, or fainting spells.
- You observe a decrease in urine production.
- Always err on the side of caution and seek the advice of healthcare professionals who can give the required care and direction.
Note:
Hospitalization may be required in severe cases of hyperemesis gravidarum. When oral intake becomes difficult, intravenous fluids can be used to replenish hydration and provide sufficient nutrition. This method allows healthcare experts to closely monitor the mother’s and developing fetus’s health.
Hyperemesis gravidarum treatments:
Managing hyperemesis requires a variety of techniques that are tailored to the needs of each individual. Among the most prevalent treatments and tactics are:
- Support for fluids and nutrition: Dehydration and nutritional imbalances are frequently treated with intravenous fluids and electrolyte replacement treatment.
- Antiemetic drugs may be used to treat nausea and vomiting. These drugs help to control the neurotransmitters that cause these symptoms.
- Nutritional changes: Working with a qualified dietitian can assist in developing a personalized dietary plan that emphasizes easy-to-digest foods and short, frequent meals.
- Complementary therapies such as acupuncture, aromatherapy, and hypnosis have been observed to provide brief relief from symptoms in certain situations.
- Remember that each woman’s experience with hyperemesis is unique, so it’s critical to speak with healthcare professionals to determine the best treatment strategy for your personal situation.
Hyperemesis Gravidarum Medication:
When it comes to hyperemesis medicine, it is critical to talk with your healthcare professional to establish the best options for you. Among the most regularly prescribed drugs are:
- Ondansetron: This drug, which can be administered orally or intravenously, helps minimize nausea and vomiting.
- Metoclopramide: This drug is used to facilitate stomach emptying and can help relieve nausea and vomiting.
- Corticosteroids: Corticosteroids may be administered in severe cases to reduce inflammation and suppress the immunological response, which contribute to hyperemesis gravidarum symptoms.
- Your healthcare practitioner will evaluate the severity of your disease and weigh the advantages and potential hazards of these medications while keeping your overall health and pregnancy in mind.
Note:
Medication may be used in some circumstances to treat the symptoms of hyperemesis gravidarum. This can include antiemetic medications that help with nausea and vomiting. However, before taking any medications during pregnancy, it is critical to check with a healthcare practitioner, as the safety of both the mother and the baby must be carefully examined.
Conclusion:
Hyperemesis is a common misdiagnosed and underdiagnosed illness that can have a substantial influence on the pregnant experience. Expectant moms can improve their chances of managing hyperemesis gravidarum and having a healthier pregnancy by recognizing its symptoms, understanding its potential causes, and obtaining appropriate therapy. Remember, if you or someone you know is suffering significant nausea and vomiting during pregnancy, it is critical that you visit with a trusted healthcare physician who can give the support and care you require to navigate this difficult path.