Preeclampsia
What is Preeclampsia?
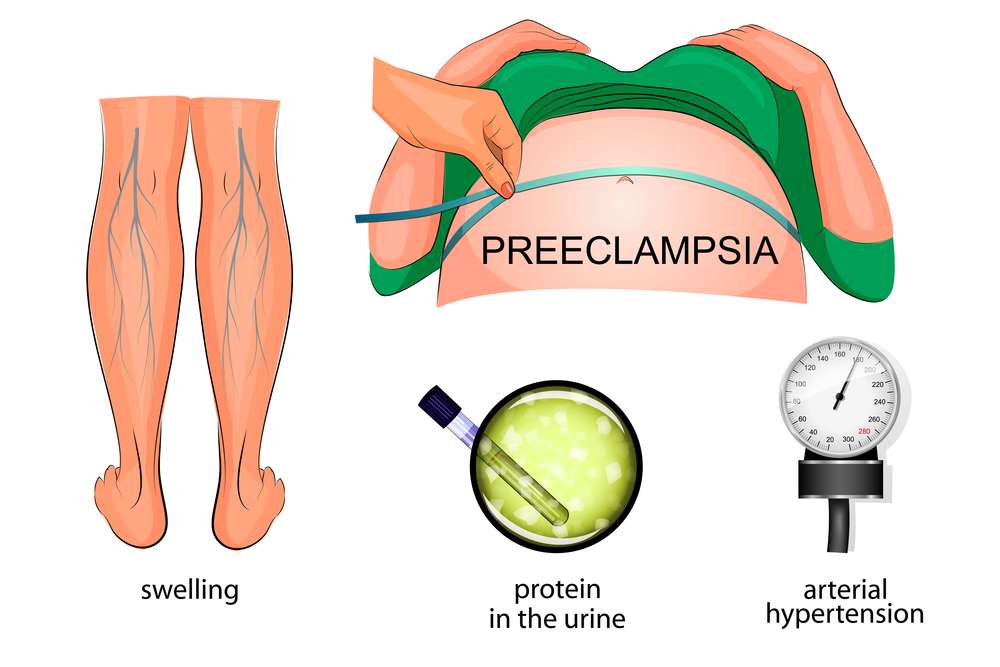
A pregnancy problem known as Preeclampsia is characterized by high blood pressure and organ damage, most frequently to the liver and kidneys. If neglected, this illness, which commonly manifests after the 20th week of pregnancy, may be fatal. It is the main factor of maternal and newborn mortality and affects 5-8% of pregnancies globally.

Symptoms of Preeclampsia
In order to discover Preeclampsia early and receive prompt medical attention, it is essential to recognize its signs. It’s important to be aware of the following symptoms even though some women may not detect any symptoms at all:
High blood pressure
Consistently raised blood pressure, typically greater than 140/90 mmHg, is a key warning indication of Preeclampsia. To correctly diagnose this illness, regular monitoring by a healthcare professional is required.
Proteinurea
The presence of protein in the urine is another sign of preeclampsia. This happens when the kidneys’ blood arteries are damaged by high blood pressure, preventing them from functioning normally. During prenatal checkups, routine urine tests can find proteinuria.
Swelling
Swelling is a very typical symptom of pregnancy, especially in the hands, face, feet, and ankles. The presence of rapid or significant edema along with weight increase, however, can indicate pre-eclampsia and should not be disregarded.
Visual disturbance and Headaches
Preeclampsia warning indications include persistent headaches that are frequently accompanied by double vision, blurred vision, or sensitivity to light. These signs should be taken seriously right away because they could point to increasing cerebral pressure.
Upper abdominal discomfort
Severe upper abdominal pain, typically under the right ribcage, may be a sign of liver involvement brought on by preeclampsia. To evaluate the problem and choose the best course of action, prompt medical care is required.
Signs of Preeclampsia
Knowing the symptoms of Preeclampsia is essential for early detection and quick medical intervention. If you have any of the following symptoms, you should contact your healthcare professional right away:
- High blood pressure (regularly greater than 140/90 mmHg)
- Proteinuria is the presence of protein in the urine.
- Hand, face, foot, and ankle swelling are common.
- Chronic headaches and visual disturbances.
- Severe upper abdominal ache, particularly beneath the right ribs
Remember that early detection and treatment of Pre-Eclampsia can improve outcomes for both you and your baby. Regular prenatal care and open conversation with your healthcare practitioner are critical for detecting any issues early.
How to treat Preeclampsia?
Once Pre-Eclampsia is discovered, it is critical to manage the illness with appropriate treatment to preserve both the mother and baby’s health. While delivery of the baby is the only definitive treatment for Preeclampsia, healthcare experts may propose the following methods to prolong the pregnancy and maintain the mother’s well-being:
Regular Blood pressure checks
Regular blood pressure checks assist healthcare personnel to determine the severity of Preeclampsia. To assist lower and regulate high blood pressure, medications may be prescribed.
Rest and activity restrictions
In more severe cases of Preeclampsia, bed rest and limited physical activity may be recommended to lessen the risk of problems and extra stress on the body.
Medications
In women with severe Preeclampsia, medications such as magnesium sulfate may be provided to avoid seizures (eclampsia). Other drugs may be administered to treat specific Preeclampsia symptoms or diseases.
Extra caution and prenatal visits
Pregnant women with Preeclampsia need more regular prenatal check-ups to closely monitor their condition and examine the baby’s health and progress. To ensure the baby’s health, additional tests such as ultrasounds and blood testing may be performed.

Preeclampsia: When to deliver?
Determining the best time for delivery is a vital decision in Preeclampsia management. Healthcare experts examine the severity of Preeclampsia, the baby’s gestational age, and the mother’s and baby’s overall health. If the Pre-Eclampsia is mild and the infant is not in immediate danger, healthcare personnel may try to postpone birth to allow for more fetal development and steroid therapy to increase lung maturity.
However, if Preeclampsia develops severe or if the mother’s or baby’s health is jeopardized, an early delivery may be required to avoid future difficulties. In such circumstances, induction of labor or cesarean section may be performed, with the mother’s and baby’s well-being being prioritized.
Preeclampsia headache location:
The location and intensity of preeclampsia headaches can vary. A persistent and pounding headache is the most common description. Here are some common characteristics of headache localization in pre-eclampsia:
- Frontal or Temporal Region: The headache is frequently described as being in the frontal (forehead) or temporal (side of the head) regions. It may affect both sides of the head or only one side.
- In many situations, the headache is bilateral, which means it is felt on both sides of the head. It can, however, be unilateral (on only one side).
- While it may begin in a localized spot, it might progress to a broad headache that affects the entire head.
- Pre-eclampsia headaches are frequently chronic and do not respond well to over-the-counter pain relievers.
Note:
While a headache can be an indication of Preeclampsia, not all headaches during pregnancy are associated with this disease. If you get a severe headache during pregnancy, especially if it is accompanied with additional symptoms such as high blood pressure, vision problems, stomach pain, or edema, you should seek medical assistance right once. These symptoms could indicate pre-eclampsia or another significant medical condition that requires immediate evaluation and management by a healthcare expert. Early detection and treatment are critical in lowering the risk of problems for both the mother and the baby.
Management of Preeclampsia:
Pre-eclampsia treatment largely consists of strict medical monitoring, blood pressure regulation, and, in certain circumstances, baby delivery. The particular management plan will be determined by the severity of the problem, gestational age, and the mother’s and baby’s overall health. Here’s a summary of pre-eclampsia treatment:
- Early and consistent prenatal care is critical for monitoring blood pressure, protein levels in the urine, and other symptoms of pre-eclampsia. This enables earlier detection and management.
- Controlling elevated blood pressure is a critical component of controlling pre eclampsia. Medication, such as antihypertensive meds prescribed by a healthcare professional, may be involved.
- Monitoring: It is critical to keep track of the mother’s and baby’s health on a regular basis. This may involve regular blood pressure checks, proteinuria urine tests, blood tests to examine organ function, and fetal monitoring to ensure the baby’s health.
- Bed rest: To control pre-eclampsia, healthcare experts may recommend partial bed rest or limited activity in some circumstances. However, full bed rest is no longer commonly prescribed because it can be harmful.
- Hospitalization: If your pre-eclampsia is severe or rapidly advancing, you may need to be admitted to the hospital for close observation and management. The length of the hospital stay will be determined by the severity of the condition and the baby’s gestational age.
- Delivery is the only permanent remedy for pre-eclampsia. If the disease is serious or worsening, and the pregnancy has reached a particular gestational age (typically about 37 weeks, or earlier in extreme situations), the healthcare professional may advise inducing labor or conducting a cesarean section (C-section) to deliver the baby and placenta.
- Corticosteroids: If pre-eclampsia is identified before the baby’s lungs are developed (typically before 34 weeks of gestation), corticosteroids may be given to help the baby’s lungs develop faster.
- Magnesium Sulfate: Magnesium sulfate may be given intravenously to prevent seizures in extreme cases of Preeclampsia or when there is a danger of seizures (eclampsia).
- Consultation with a Specialist: In severe or complex instances, a maternal-fetal medicine specialist, a high-risk pregnancy specialist, or a multidisciplinary team of healthcare specialists may be required.
- Postpartum Care: Even after delivery, blood pressure and other health indicators must be monitored and managed, as some preeclampsia issues might persist or worsen.
- Pregnant women must attend all prenatal checkups, follow their healthcare provider’s advice, and be aware of the signs and symptoms of Preeclampsia. Early detection and quick care are critical for both the mother and the baby’s health. If you suspect you have preeclampsia or have any concerns during your pregnancy, you should contact your healthcare professional right away.
Where is Preeclampsia pain?
Preeclampsia does not usually cause particular localized pain. Instead, it is distinguished by a slew of symptoms that might affect diverse sections of the body. While pain is not the major symptom of preeclampsia, the following are some symptoms and discomforts that are typically connected with the condition:
- Many women with pre eclampsia develop persistent, often severe headaches in the frontal (forehead) or temporal (side of the head) areas. The severity of these headaches can vary.
- Some preeclamptic women may suffer upper abdominal pain, mainly on the right side, under the ribs. This could indicate liver involvement
- Preeclampsia can cause severe swelling, particularly in the hands, feet, and face. While this swelling can be bothersome, it is usually not painful.
- Preeclampsia can induce visual disturbances such as blurred vision, spots, or flashing lights, which can be disturbing but are not always uncomfortable.
- Pre eclampsia can induce fluid buildup in the lungs, resulting in shortness of breath or trouble breathing in extreme cases.
- Pre eclampsia can also induce a general feeling of being unwell or discomfort, which may not be confined to a specific place.
- It’s crucial to remember that, while pain isn’t the only sign of preeclampsia, the illness can be fatal if left untreated. If you feel you have pre eclampsia, consult your doctor.
What is Postpartum Preeclampsia?
Postpartum pre-eclampsia is a disorder in which preeclampsia symptoms, such as high blood pressure and often proteinuria (excess protein in the urine), arise after the birth of a baby. This syndrome manifests itself during the postpartum period, usually between the first 48 hours to six weeks after childbirth. It is distinct from preeclampsia, which occurs during pregnancy. Here are some important facts to remember concerning postpartum preeclampsia:
- Symptoms: Postpartum preeclampsia has symptoms that are similar to preeclampsia during pregnancy.
- High blood pressure (hypertension), headache, visual problems, swelling (edema), abdominal pain, and proteinuria (excess protein in the urine) are some of the symptoms.
- Factors of Risk: While postpartum preeclampsia can occur in women who have no history of hypertension or preeclampsia during pregnancy, it is more likely in women who have a history of hypertension or Preeclampsia during pregnancy.
- Diagnosis is based on the existence of symptoms as well as clinical examinations such as blood pressure monitoring and urine testing to rule out proteinuria.
- Treatment: Postpartum preeclampsia is treated similarly to preeclampsia during pregnancy. It usually entails blood pressure medicine, such as antihypertensive medications. Hospitalization and intravenous medicines may be required in extreme situations. The delivery of the placenta following childbirth usually helps to resolve the condition, but medical therapy is still necessary.
- Monitoring: It is critical to keep a close eye on the mother’s blood pressure and other vital signs. Healthcare practitioners will also evaluate organ function to ensure that issues such as renal or liver disease are addressed as soon as possible.
- Breastfeeding: Women with postpartum preeclampsia can usually continue breastfeeding, but it’s important to check with your doctor to be sure any drugs you’re taking are compatible with breastfeeding.
- Follow-up care is required after the initial treatment to check blood pressure and confirm the issue has resolved.
- Postpartum preeclampsia can occur abruptly and can be a significant medical disease if not detected and treated properly. Individuals who have recently given birth must be aware of the signs and symptoms of pre eclampsia and seek prompt medical assistance if any alarming symptoms occur. Early intervention and adequate treatment are critical for the mother’s health.
Preeclampsia 32 weeks:
Preeclampsia during 32 weeks of pregnancy is a dangerous medical disease that necessitates immediate medical treatment and management. The infant is considered preterm at this time of pregnancy, which complicates the management and care of both the mother and the baby. What you should know about preeclampsia at 32 weeks:
- Diagnosis: High blood pressure (usually defined as systolic blood pressure 140 mm Hg or diastolic blood pressure 90 mm Hg on two separate readings at least 4 hours apart), proteinuria (excess protein in the urine), and other signs of organ dysfunction are used to diagnose preeclampsia.
- If pre eclampsia is identified at 32 weeks, both the mother and the baby will need to be closely monitored. Regular blood pressure checks, urine tests, and fetal monitoring are all part of assessing the baby’s well-being.
- Prescription drugs: Depending on the severity of preeclampsia, healthcare experts may prescribe medications to reduce blood pressure and prevent problems. To manage high blood pressure, medications such as antihypertensive medicines may be prescribed.
- Corticosteroids: Corticosteroids are commonly used to enhance fetal lung development in situations of preeclampsia at 32 weeks or earlier. This is because preterm labor may be required to protect the mother’s health.
- Hospitalization may be required in severe cases of pre-eclampsia for closer monitoring and management.
- Preeclampsia is eventually addressed by delivering the baby and the placenta. The severity of pre-eclampsia, the baby’s gestational age, and the overall health of both the mother and the baby will all influence the timing of birth. In some situations, labor may need to be induced or delivered via C-section.
- Neonatal Care: Babies born at 32 weeks are considered preterm and may require specialist care in the neonatal intensive care unit (NICU) to manage any potential prematurity issues.
Postpartum Care: It is critical to continue monitoring the mother’s blood pressure and overall health after delivery, as some preeclampsia issues can remain or develop after childbirth. - Pre-eclampsia at 32 weeks is a high-risk situation that requires collaborative care from obstetricians, neonatologists, and other healthcare specialists. The goal is to protect the mother’s and baby’s safety and well-being. Close communication with the healthcare staff and following their advice are critical for the best potential results.
Conclusion:
Preeeclampsia is a dangerous medical condition that can occur during pregnancy, usually after 20 weeks. It is distinguished by high blood pressure (hypertension), proteinuria (extra protein in the urine), and, in certain cases, organ damage, including as damage to the liver and kidneys. Preeeclampsia can cause a variety of symptoms and consequences, and its treatment is determined by factors such as the severity of the condition, gestational age, and the overall health of the mother and baby.



Pingback: Postpartum Preeclampsia - Journey Of Mother
Pingback: Cramps During Pregnancy - Journey Of Mother