Gestational diabetes
Introduction:
Gestational diabetes is a transient illness that emerges during pregnancy and affects women who have never had diabetes before. In order to support a healthy pregnancy, it is critical to understand this condition and its implications for both the mother and the baby. In this post, we will look at the symptoms, causes, testing methods, treatment choices, and preventive measures of gestational diabetes.
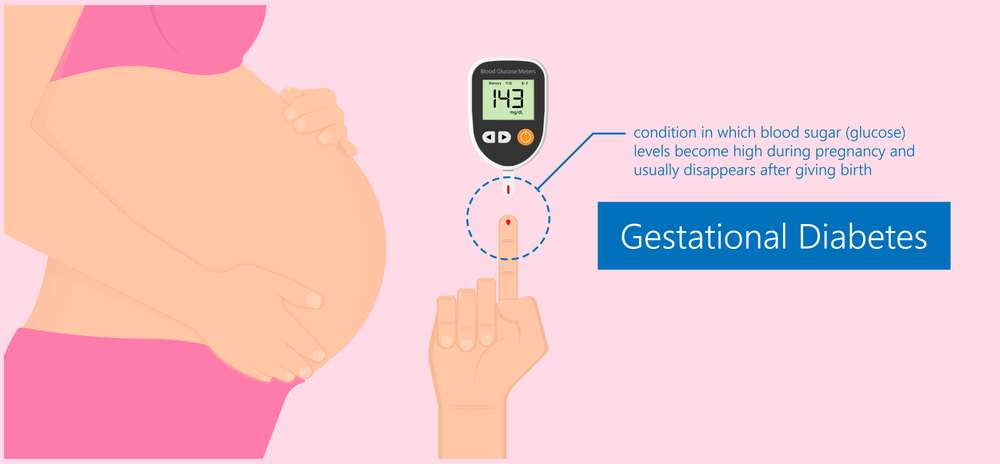
What is Gestational diabetes?
Gestational diabetes is a kind of diabetes that occurs during pregnancy, most commonly between the 24th and 28th week. When the body is unable to manufacture and utilise insulin adequately, it results in high blood sugar levels. Unlike other types of diabetes, gestational diabetes normally goes away after the baby is born.
What causes Gestational diabetes?
The exact origin of diabetes is unknown, although the following variables enhance the likelihood of having the condition:
- Changes in hormones
- Various hormones can interfere with insulin activity during pregnancy, resulting in gestational diabetes.
- Insulin sensitivity
- Some women are born with cells that do not respond well to insulin, rendering them more vulnerable to gestational diabetes.
- Excessive gaining of weight
- Excess weight before and during pregnancy increases the risk of acquiring gestational diabetes.
- Family history
- Having a close family member with diabetes, such as a parent or sibling, can increase the risk of gestational diabetes.
Gestational diabetes test:
A glucose screening test is frequently recommended by healthcare providers to determine gestational diabetes. A fasting blood sugar test is performed, followed by the consumption of a high-glucose drink. After an hour, blood sugar levels are measured with a blood sample. If the findings show that the levels are greater than usual, a follow-up glucose tolerance test may be done.
Gestational diabetes Treatment:
When an expectant mother is diagnosed with diabetes, healthcare specialists will work closely with her to control the disease. Among the treatment options available are:
- Dietary changes
- Adopting a well-balanced meal plan that limits carbohydrate intake can aid with blood sugar management.
- Exercise on a regular basis
- Physical exercises including as walking or prenatal yoga can help manage blood sugar levels.
- Monitoring of blood sugar levels
- Regularly testing blood sugar levels and noting the results aid in tracking treatment efficacy.
- Medication, if required
- To help regulate blood sugar levels, insulin injections or oral medicines may be administered in some circumstances.
Gestational diabetes symptoms:
Identifying gestational (diabetes) symptoms is critical for early detection and adequate care. Although some women have no discernible symptoms, others may exhibit the following:
- Urination on a regular basis
- Urinating more frequently could indicate high blood sugar levels.
- heightened thirst
- Excessive thirst can suggest elevated blood sugar levels, which should be investigated further.
- Fatigue
- A persistent feeling of exhaustion may be connected with gestational diabetes.
- Vision distortion
- Elevated blood sugar levels can cause vision changes such as blurred vision.
- Infections that reoccur
- Women who have gestational diabetes are more likely to get urinary tract infections or yeast infections.
Signs of Gestational diabetes:
In addition to the signs listed above, healthcare practitioners look for the following markers when diagnosing gestational (diabetes):
- High blood sugar levels
- Blood testing can tell healthcare practitioners whether blood sugar levels are greater than normal.
- Increased pregnancy weight gain
- Rapid pregnancy weight gain can alert clinicians to the likelihood of gestational diabetes.
- Baby size that is larger than typical
- An ultrasound may demonstrate that the baby is larger than normal for the stage of pregnancy, indicating the possibility of gestational diabetes.
Gestational diabetes range:
When blood sugar levels rise above certain limits during pregnancy, diabetes is diagnosed. The following ranges are commonly used for diagnosis:
- Blood sugar level after fasting: more than or equal to 92 mg/dL
- Blood sugar level one hour after glucose drink: equal to or more than 180 mg/dL
- Blood sugar level two hours after glucose drink: equal to or more than 153 mg/dL
Gestational diabetes Meal plan:
Following a well-structured diet plan is critical for diabetes management. Consider the following recommendations:
- Carbohydrates should be balanced.
- Choose healthy grains, fruits, and vegetables over refined sugars and processed foods.
- Include some lean protein.
- Include lean protein sources in your meals, such as poultry, fish, tofu, and lentils.
- Concentrate on good fats.
- Avocado, almonds, and olive oil are all examples of healthy fats that can supplement your diet.
- Keep an eye on portion sizes.
- To avoid excessive carbohydrate intake and blood sugar increases, keep portion sizes in mind.
Gestational diabetes medication:
When diet and exercise alone are ineffective at controlling blood sugar levels, medication may be required. To help manage gestational (diabetes), healthcare providers may prescribe insulin injections or oral medicines like as metformin. Before beginning any pharmaceutical regimen, contact with your healthcare physician.
Gestational diabetes Self care:
While healthcare providers play a significant role in gestational (diabetes) management, self-care is equally important. Think about the following self-care practices:
- Check your blood sugar levels on a regular basis.
- Follow the diet and exercise plan that has been prescribed.
- Keep all prenatal appointments.
- If emotional help is required, seek it.
- Relaxation practices might help you control your stress levels.
How to Prevent Gestational Diabetes?
While it is not always possible to avoid gestational diabetes, various lifestyle changes can lessen the risk:
- Maintain a healthy weight before becoming pregnant.
- Participate in frequent physical activity.
- Maintain a well-balanced diet.
- If you are at high risk, keep a close eye on your blood sugar levels.
- Discuss any concerns you have with your doctor.
How Common is Gestational Diabetes?
Gestational diabetes is relatively prevalent, affecting 6-9% of pregnant women. It is critical to remember that women with diabetes can have healthy babies with careful management and attention to healthcare provider guidelines.
How to Avoid Gestational Diabetes?
Consider the following preventive actions to avoid the potential problems of gestational diabetes:
- Make healthy lifestyle choices before you become pregnant.
- If you are at high risk, keep a close eye on your blood sugar levels.
- Seek advice from a healthcare expert on the best prenatal vitamins and supplements for you.
- Attend prenatal check-ups on a regular basis to monitor any changes or developments.
What Happens If You Have Gestational Diabetes?
It is critical to remain proactive if you have gestational diabetes:
- Follow the treatment plan that has been prescribed.
- Regularly check your blood sugar levels.
- Attend all of your prenatal checkups.
- Inform your healthcare practitioner of any concerns or changes.
- If emotional help is required, seek it.
How Does Gestational Diabetes Affect the Baby?
Gestational diabetes can have a variety of effects on the baby’s health, including:
- Risk of macrosomia has increased.
- Babies born to diabetic moms may develop larger than typical, resulting in problems during delivery.
- Hypoglycemia upon birth
- Due to exposure to greater glucose levels in the pregnancy, the baby may develop low blood sugar after delivery.
- Future type 2 diabetes risk is increased.
- Babies born to moms who have gestational (diabetes) are more likely to develop type 2 diabetes later in life.
What to Eat With Gestational Diabetes?
When dealing with gestational diabetes, it is critical to eat a balanced and healthy diet. Consider including the following foods in your diet:
- Foods high in fiber
- Whole grains, fruits, and vegetables are high in fiber, which helps to keep blood sugar levels stable.
- Proteins that are low in fat
- Chicken, turkey, fish, tofu, and lentils are all low in fat and high in nutrients.
- Fats that are good for you
- Avocados, nuts, seeds, and olive oil include healthful fats that contribute to a well-balanced diet.
How to Treat Gestational Diabetes?
Treatment for gestational (diabetes) often consists of a mix of dietary changes, physical activity, regular blood sugar monitoring, and medication (if necessary). To properly manage the disease, always follow your healthcare provider’s advice and seek help.
Risk of gestational diabetes:
Diabetes that occurs during pregnancy is known as gestational (diabetes). It is distinguished by elevated blood sugar levels that develop or are discovered during pregnancy. While gestational diabetes is a common illness, there are some risk factors that can enhance a woman’s chances of having it. These are some of the risk factors:
- If you have a family history of (diabetes), especially a close relative such as a parent or sibling, you may be at a higher risk.
- Age: Women over the age of 25, in general, are at a higher risk.
- Obesity: Being overweight or obese prior to pregnancy raises the chances of developing gestational diabetes.
- Previous Gestational Diabetes: If you had gestational diabetes in a previous pregnancy, your risk of developing it again in subsequent pregnancies is increased.
- Polycystic Ovary Syndrome (PCOS): Women who have PCOS are more likely to develop gestational diabetes.
Ethnic groups with an increased risk of gestational diabetes include African-Americans, Hispanics, Native Americans, and Asian-Americans. - High Blood Pressure: Your risk may be increased if you have high blood pressure (hypertension) before or during pregnancy.
- Excessive Amniotic Fluid: Having too much amniotic fluid (polyhydramnios) can raise your risk of gestational diabetes.
- Gestational Diabetes in a Previous Pregnancy: If you’ve previously had gestational (diabetes,) you’re more likely to get it again in subsequent pregnancies.
It’s crucial to remember that having one or more risk factors doesn’t guarantee you’ll have gestational (diabetes,) and women who don’t have any of these risk factors can still get the illness. Furthermore, gestational diabetes usually resolves after pregnancy. However, gestational diabetes must be managed and monitored during pregnancy in order to reduce the dangers to both the mother and the baby.
If you are pregnant or expecting to get pregnant and are concerned about gestational (diabetes,) talk to your doctor about your risk factors. They can advise you on how to monitor and manage your blood sugar levels during pregnancy in order to have a healthy pregnancy and delivery.
How to control Gestational diabetes?
To ensure a healthy pregnancy and limit the risk of complications for both the mother and the baby, gestational diabetes must be managed. Here are some key strategies for gestational (diabetes) management:
- Blood sugar levels should be checked on a regular basis. Your doctor would most likely advise you to check your blood sugar levels on a frequent basis. Checking your fasting blood sugar level in the morning and your blood sugar level one to two hours after meals is typical. Maintaining a record of your readings can assist you and your healthcare team in determining how well your blood sugar is controlled.
- Plan for a Healthy Diet: Follow the diet recommendations of a licensed dietician or healthcare provider.
- Eating at Regular Intervals: Aim for three meals and two to three snacks each day to help maintain blood sugar levels.
- Balancing Carbohydrates: Be mindful of the type and quantity of carbohydrates you ingest. Complex carbs with a low glycemic index are usually preferable.
- Portion Management: Control portion amounts to avoid overeating, which can trigger blood sugar rises.
- Sugary Foods to Avoid: Reduce or eliminate sugary meals and beverages from your diet.
- Fiber is included: Include high-fiber items in your diet, such as whole grains, fruits, and vegetables.
- Regular Physical Activity: Moderate physical activity, like as walking, swimming, or prenatal yoga, can assist in lowering blood sugar levels. Before beginning or continuing any fitness routine, consult your healthcare practitioner and follow their recommendations.Medication or Insulin Therapy: Lifestyle adjustments alone may not be enough to control gestational diabetes in some circumstances. To assist regulate your blood sugar levels, your doctor may recommend medication or insulin therapy.
- Attend all of your prenatal checkups since your healthcare professional will regularly monitor your pregnancy and the baby’s growth. They will also assess your blood sugar control and, if necessary, change your treatment strategy.
- Stress Reduction: Blood sugar levels can be affected by high levels of stress. Deep breathing, meditation, and mindfulness are among relaxation practices that can help reduce stress during pregnancy.
- Joining a support group or seeking help from family and friends might be beneficial. Sharing your worries and experiences with others who have or are experiencing gestational diabetes can provide emotional support as well as useful advice.It is critical to follow the instructions and guidelines provided by your healthcare team. This may include routine examinations, blood sugar monitoring, and sticking to your treatment plan.
Note:
Remember that gestational (diabetes) usually resolves after pregnancy, but treating it throughout pregnancy is critical for your and your baby’s health. Consult your healthcare practitioner and a trained dietitian to develop a personalized plan that suits your individual needs and assists you in effectively controlling gestational diabetes.
Conclusion:
Gestational (diabetes) is a short-term condition that requires close monitoring and control during pregnancy. Expectant moms can take proactive care of themselves and their newborns if they understand the symptoms, causes, and treatment choices. Remember to seek correct diagnosis and individualized guidance from healthcare professionals to ensure a healthy and successful pregnant experience.




Pingback: Glucose Test Pregnancy - Journey Of Mother